Rama Medical College, Hospital and Research Centre, Ghaziabad, UP, India.
Aim of the Study: To compare the effect of open and closed method in burn dressing respect to various parameters of healing.
Method: In the open method of dressing antiseptic ointment was applied all over the burnt area after all dead tissue and blisters were removed. Patients were kept covered with two sterile / washed bed sheets one below and one above the patient. The bed sheets were washed daily and changed. In the closed dressing group patients were washed with jet spray of diluted beta-dine solution and thoroughly washed with normal saline. All dead tissue and blisters were removed. Antiseptic ointment was applied and dressing was done in three layers. First layer with sterile gauze, second absorbent cotton pads and third layer pressure bandaging with gauze.
Result: Appearance of granulation tissue was almost similar in open and closed dressing where as epithelization was earlier in open dressing then in closed dressing.
Conclusion: It is concluded that open method was superior to closed dressing method especially in patients with less extensive burns of extremities particularly in children, who could not be easily controlled in cradles in patient of superficial to deep burns involving front and back and chest. Facial burns were treated by exposure method which helps in taking care of eyes, ear and nose.
Keywords: burn wound, open dressing, closed dressing
Burn is a serious traumatic wound produced by thermal energy or chemical substances upon the protective covering of the body, damaging the underlying tissues.[1] The wound ranges from microscopic destruction at cellular level in first degree burn to complete coagulation of all layers of skin. Burn wound is a catastrophy. It affects the psychology of patients & the cost & suffering to family is also a issue for concern. The wound healing process is a complex biological process leading to adequate surfacing the structural continuity & strength approximating normal tissues. In superficial burns a certain thickness of epithelial tissue is still intact & it will give full regeneration of skin. In deep burns complete loss of skin occurs which heals by secondary intention due to which scarring may results producing disabilities & disfigurements.[1],[2] Any kind of biological or synthetic dressing has a role in decreasing pain, decreasing protein loss, reducing the evaporative heat & water loss from the wound a guard against secondary infections & protect the viable epithelium from destruction & also provides a scaffolding for epithelial in growth. The dressing method is accepted worldwide.[3],[4] The exposure method or open method of burn dressing also enjoys acceptance because of its simplicity, ease of examination of burn wound, daily debridement, physical therapy & willingness to change the therapy when Escher begin to separate. Also these do not interfere with heat loss esp. in warm months of the year.[5],[7] The Escher which forms over the burnt area serves as a biological dressing, maintaining the warmth preventing water evaporation & also prevents the bacterial growth over it from reaching the systemic circulation.[7],[8] The Escher separates in about 4-5 weeks when healthy granulation tissue has developed underneath it. Exposure method is also excellent form of treatment for mass causalities when limited medical staff curtails the use of bulky dressings.[9]
The present study was carried out in 464 patients admitted in surgical ward and burn unit, Department of General Surgery, K.D. Medical College & Hospital Mathura (UP) during the period of May 2016 to November 2016. The study includes patients of burns who were admitted through surgical OPD or casualty Department. On admission preliminary enquiries were made. General & systemic examinations were performed to find out any associated problem
Selection criteria of patient for open dressing were involved the Superficial burn involving face and neck; Superficial burn involving anterior wall chest and abdomen; Superficial burn area less than 10% of extremities; Superficial burn perineum; Body surface area less than 20% involved from different part of body.
In the open method of dressing antiseptic ointment was applied all over the burnt area after all dead tissue and blisters were removed. Patients were kept covered with two sterile/washed bed sheets one below and one above the patient. The bed sheets were washed daily and changed. The patients were kept in a cradle covered with mosquito nets or bed sheets. The cradles were either metallic made of steel or just supporting bamboo sticks attached to the edges of the bed. The patients were encouraged to take daily baths followed by examination and debridement of wound which was done accordingly. Selection criteria of patient for closed dressing were involved the Deep burn involving extremities; Superficial to deep burn in both side chest abdomen; Deep burn involving body surface less than 20%; Patient treated with open method developing oedema, oozing and pain.
In the closed dressing group patients were washed with jet spray of diluted betadine solution and thoroughly washed with normal saline. All dead tissue and blisters were removed. Antiseptic ointment was applied and dressing was done in three layers. First layer with sterile gauze, Second layer was absorbent cotton pads and Third layer with pressure bandaging with gauze. Dressing was changed every 3rd or 4th day, examination was performed and debridement done accordingly.
The state of the wound was observed & compared every 3rd day and following points were noted: Pain present or absent; Escher removal started or not; Pus discharge present or absent; Granulation tissue started to develop or not; Epithelization of wound started or not; Complications if present and these were managed accordingly.
Patients were discharged when they recovered from the primary shock. Patients who had superficial burns with involvement of less than 10 %, involving the extremities or face without involvement of eye or ear were discharged with continuation of oral antibiotic remaining tetanus prophylaxis and dressing at their residence with advise for follow up in surgery OPD.
Other patients were discharged either on request or who had facilities for dressing at nearby medical centers or/and referred to other centers where facilities for primary skin grafting or surgical correction of developing deformities was present.
Table 1: Distribution of cases based on the Persistence of Pain after burns in Open and Closed Dressing Method (n=464)
It is evident from the table 1 that pain was recorded from 1st to 3rd days in majority of patient of both groups. Some patient could not appreciated pain under the effect of analgesics and sedatives. It is clear that in case of exposure method of treatment pain persist even after 10 days as compare to group of closed dressing were it was persist for 8 days.

Table 2: It is evident from table 2 that maximum number of burn cases had burn over lower limb i.e. 30.38% and minimum burn cases recorded over genital region i.e. 4.52%. Over head and neck region out of 33 cases 29 cases kept over open dressing.

Table 3: Distribution of cases according to condition of wound on discharge on aspect of open and closed dressing
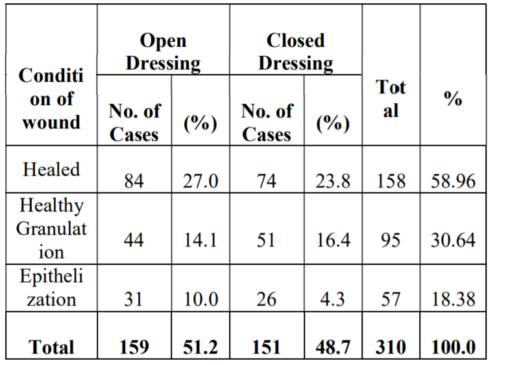
It is evident from table 3 that more cases of epithelization in open dressing i.e. 10% where as in closed dressing it was 8.38% of cases found. Healthy granulation tissue found in 44 cases in open dressing i.e. 14.19% where as it was 51 cases in closed dressing i.e. 16.45%.
Table 4: Distribution of cases according to development of complication in aspect of open and closed dressing

It is evident from table 4 that more number of cases found epithelization in open dressing i.e. 55.9% but in closed dressing it was less i.e. 44.80%. More number of epithelization was found in open dressing i.e. 20.77% but it was of 16.88% in closed dressing. Hypergranulation tissue was found in 25 cases i.e. 16.23% but it was 13.63% in closed dressing.
The burn is a serious traumatic wound produced by excessive heat upon the protective covering of body, damaging the underlying tissues causing circulatory disturbances and mild or severe constitutional disturbances. If untreated burn injuries results in intense suffering and protracted course of illness possible disfiguration with psychological trauma to patients, cost and sufferings to the family involved. Care of local burn wound has drawn attention of many workers worldwide. Many differences of opinion are prevailing. Most surgeons use all methods and all methods are acceptable and available. It is up to the surgeon to select the one which is most desirable for a particular patient and at a particular time.[10]
There are three methods of treating wound of burns and scalds – open or exposure method, closed dressing method and primary excision with skin grafting. In our study, we used closed method of dressing in 93 patients, and 87 patients had received exposure method. Patients of all ages were equally studied for both method of dressing so that any bias could be avoided. Open or exposure method as popularized by Haldor Sneve of St. Paul in 1905 permits frequent examination of wounds, daily debridement, physical therapy and early detection of infection. One of the disadvantages of this method is increased duration of pain. As is evident from table majority of patients of open dressing method reported pain upto 9 days, where as patients of closed dressing method get pain relief usually within 6 days.[11]
By the end of first week, pus begins to form in the wounds. In the closed method pus begins to form as early as fourth day of admission where as in open method pus formation is delayed in majority of patients for up to one week this is in conjunction to the findings of one study in which he noticed that dryness and coolness are factors that are unfavorable to the growth of pyogenic organisms. The edema of burn wounds begin to subside by the end of first week after burn. As evident from table that edema disappeared equally in both the groups and type of dressing had no major effect on subsidence of edema. By the end of second week after burn the eschar begins to separate. In our present series we noticed that removal of eschar begins earlier in closed dressing method, usually between 7-9 days as compared to the open dressing group in which it usually start by 10-14 days. This is because moistness and exudation in closed dressing group liquefies and separates the eschar along with the change of dressing. In the open dressing method eschar remains dry and adhered to the surface and begins to separate only when pus develops underneath its surface.[12]
As soon as the eschar separate granulation tissue starts appearing over the surface in our series appearance of granulation tissue was a bit earlier in open dressing group (15.6 days) as compared to closed dressing group (16.5 days). This is due to greater pus formation and sloughing in closed dressing group resulting increased time for appearance of healthy granulation. Artz and Moncrief (1969) had reported similar findings that deep dermal burns treated by open method became dry and usually healed uneventfully, however when treated by closed dressing method they became infected and converted to full thickness burns.[11],[12]
One of the major determinants of healing is epithelisation. In our series we noticed that epithelial tissue appears earlier in open dressing method as compared to closed dressing group. In open method epithelial tissue appears on an average on the 17th day whereas in closed method it is noticed around the 21st day. One reported study found found that most important advantage of exposure treatment was decreased hospitalization time. In our series too, time of hospitalization are less for each extent of burns surface area in open as compared to closed dressing group with a mean of 17 days in open method and 21 days in closed method. When we see the mortality in cases according to the method of dressing adopted we find that mortality rate was a bit higher in closed dressing method for up to 40% extent of wound as compared to open method. Above 40% extent of burn mortality was significantly higher in closed dressing method but this was because most of the cases were treated by this method only and hence comparison is not possible. Finally we can conclude that open method is a low cost alternative in our setting. It gives better results as far as healing and hospitalization are concerned. Although the problem of persist pain and unsightly appearance remains same. Closed dressing is equally recommended because poorly isolated wards, absence of temperature regulation, decreased cross contamination, decreased pain and increased comfort to patients are its positive points.[13],[14]
Patients were resuscitated and burn wound were treated by open and closed dressing. In open dressing criteria were superficial burn involving face and neck, anterior wall chest and abdomen, burn area less than 10% of extremities and burn over perineum. In closed dressing criteria were Deep burn involving extremities, superficial to deep burn in both side chest and abdomen, deep burn involving body surface less than 20% and patient treated with open method developing edema, oozing and pain. Wounds were observed and healing were recorded subjective changes in the patients in relation to pain, presence of granulation tissue, pus discharge or epithelization were recorded. Patients who were discharge or expired within 7 days were excluded under study, After reviewing relevant literatures, observations were systematically recorded, critically analysis and following conclusions were drawn:-
Healing of burn wound was studied in total of 464 patients of burn after exclusion of the cases. Burn wound was managed by closed dressing method in 241 patients and by open method in 223 patients. Patients of all age group were taken into the study and compared with respect to pain relief, pus discharge, subsidence of edema, Escher removal, appearance of granulation tissue and epithelisation. Majority of patients of opened dressing group get pain persist for 4-6 day(42.60%).whereas in close dressing pain persist for 0-3 days(50%). Patients of opened dressing group get pain persist 10-12 days (5.80). Whereas in closed dressing group pain persisted for 10-12 day in 1.2% of patients. It is clear that in case of exposure method of treatment pain persist even after 10 days as compare to group of closed dressing were it was persist for 8 days
Appearance of granulation tissue is quite earlier in patients of open dressing group when we compare the mean of number of days and we find that the mean time interval for proliferation of granulation tissue in open method was 15.6 days and in closed dressing group the mean time interval was 16.47 days. Epithelisation also started earlier in patients of open dressing group on an average on the 17th day as compared to closed dressing group in which it started on 21st day.
Pain in more pronounced in open dressing group then in patients of closed dressing method and patients of closed methods get pain relief earlier (within 6 days) as compared to open dressing method in which pain can persist for up to 9 days. It is concluded that open method was superior to closed dressing method especially in patients with less extensive burns of extremities particularly in children, who could not be easily controlled in cradles in patient of superficial to deep burns involving front and back and chest. Facial burns are treated by exposure methods which help in taking care of eyes, ear and nose.
Open method has less pus discharge less problem of foul odours, early epithelisation and shorter hospital stay. It has the simplicity in care and dread of frequent change of dressing especially in extensive burns is eliminated. Open method is also quite suitable for mass casualties where limited man power does deserve a concern. The closed dressing method does avoid the ghastly appearance of the patient to the attendants, prevents cross contamination need for temperature regulation and isolation, decreased pain and suffering to the patient and is also quite comfortable. Decreased heat loss, decreased wound desiccation and self debriding effect makes it quite useful for a set up.
References
- 1.NW Law, H Ellis. Exposure of the wound: Safe economy in the NHS. Postgrad Med J. 1987;63:27– 28. [Google Scholar] [PubMed]
- 2.A Asnake. A comparison of exposed with closed method of management of clean abdominal surgical wounds. ECAJS. 2001;6(2):21–24. [Google Scholar] [PubMed]
- 3.O Katakura, N Morimoto, Y Iwasaki, K Akiyoshi, S Kasugai. Evaluation of 2-methacryloyloxyethyl phosphorylcholine (MPC) polymer-coated dressing on surgical wounds. J Med Dent Sci. 2005;52(2):115–21. [Google Scholar] [PubMed]
- 4.OM Alvarez, PM Mertz, WH Eaglstein. The effect of occlusive dressings on collagen synthesis and reepithelialization in superficial wounds. J Surg Res. 1983;35:142–48. [Google Scholar] [PubMed]
- 5.D Demetriades, G Psaras. Occlusive versus semiopen dressings in the management of skin graft donor sites. SA fr Surg. 1992;30(2):40–41. [PubMed] [Google Scholar] [PubMed]
- 6.RC Burton. Postoperative wound infection in colonic and rectal surgery. Br J Surg. 1973;60(5):363–65. [Google Scholar] [PubMed]
- 7.AK Deodhar, RE Rana. Surgical physiology of wound healing: a review. J Postgrad Med. 1997;43(2):52–56. [Google Scholar] [PubMed]
- 8.LM Mioton, SW Jordan, PJ Hanwright, KY Bilimoria, JY Kim. The Relationship between Preoperative Wound Classification and Postoperative Infection: A Multi- Institutional Analysis of 15,289 Patients. Arch Plast Surg. 2013;40(5):522–29. [Google Scholar] [PubMed]
- 9.PJ Cruse, R Foord. A five-year prospective study of 23,649 surgical wounds. Arch Surg. 1973;107:206–10. [Google Scholar] [PubMed]
- 10.PJ Cruse, R Foord. The epidemiology of wound infection: a 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27–40. [Google Scholar] [PubMed]
- 11.EM Ferraz, TS Bacelar, JL Aguiar, AA Ferraz, G Pagnossin, JE Batista. Wound infection rates in clean surgery: a potentially misleading risk classification. Infect Control Hosp Epidemiol. 1992;13(8):457–52. [Google Scholar] [PubMed]
- 12.CJ Walter, JC Dumville, CA Sharp, T Page. Systematic review and meta-analysis of wound dressings in the prevention of surgical-site infections in surgical wounds healing by primary intention. Br J Surg. 2012;99:1185–94. [Google Scholar] [PubMed]
- 13.A Quirinia, A Viidik. The influence of dressing on the healing of normal and ischaemic wounds and flap survival. Scand J Plast reconstruct Surg Hand Surg. 2001;35:1–6. [Google Scholar] [PubMed]
- 14.SA McGarry, JJ Engemann, K Schmader, DJ Sexton, KS Kayen. Surgical-site infection due to Staphylococcus aureus among elderly patients: mortality, duration of hospitalization, and cost. Infect Control Hosp Epidemiol. 2004;25:461–7. [Google Scholar] [PubMed]