Department of Pharmacology, College of Medicine, Shaqra University, Shaqra-11961, Saudi Arabia.
Alzheimer’s disease (AD) is a progressive and fatal dementia of unknown cause characterized by loss of cognitive and physical functioning, commonly with behavior or noncognitive symptoms. Noncognitive symptoms associated with Alzheimer’s disease and related dementias consist of mood sisterbances, psychosis, altered sexual behavior, personality changes, agitation, aggression, pacing, wandering, , changed sleep patterns, and appetite disturbances. These noncognitive symptoms of dementia are common, disabling to both the patient and the carer. physicians will often play a major role in diagnosing and treating dementia and related disorders in the community. Accurate treatment of noncognitive symptoms is important. Accordingly, we reviewed the available pharmacotherapy in the clinical management of noncognitive symptoms of dementia.
Non-cognitive symptoms are described as neuropsychiatric symptoms or ‘behavioural and psychological symptoms of dementia’ (BPSD), terms that include delusions, hallucinations, depression, anxiety, apathy and a range of behaviours, such as aggression, wandering, disinhibition and agitation. It is suggested that these behaviours may occur in up to 90% of people with AD.[1]-[3] The noncognitive symptoms of dementia are not only distressing and, at times, dangerous for the patient with dementia, but also confer a high degree of burden to those charged with caregiving. Furthermore, psychiatric symptoms of dementia have been found to increase rates of institutionalization and overall financial costs. Successful intervention with behavioral and pharmacologic therapies may help to delay nursing home placement and improve the quality of life for the individual with dementia and their caregivers. [4]-[7]
Pharmacotherapy for noncognitive symptoms targets psychotic symptoms, inappropriate or disruptive behavior, and depression. Medications and recommended doses are shown in Table 1 and medication to tragets the symptoms are shown in Table 2.
TGeneral guidelines include the (1) Use environmental interventions first and pharmacotherapy only when necessary; (2) identify and correct underlying causes of disruptive behaviors when possible; (3) start with reduced doses and titrate slowly; (4) monitor closely; (5) periodically attempt to taper and discontinue medication; and (6) document carefully. Avoid anticholinergic psychotropic medications as they may worsen cognition.[8]-[10]
Cholinesterase inhibitors and memantine have shown modest improvement of behavioral symptoms over time but may not significantly reduce acute agitation. [11],[12]
Antipsychotic medications have traditionally been used for disruptive behaviors and neuropsychiatric symptoms, but the risks and benefits must be carefully weighed. A meta-analysis found that only 17% to 18% of dementia patients showed a modest treatment response with atypical antipsychotics. Adverse events (eg, somnolence, extrapyramidal symptoms, abnormal gait, worsening cognition, cerebrovascular events, and increased risk of death) offset advantages. Another systematic review and meta-analysis found small but significant improvement in behavioral symptom scores in patients treated with aripiprazole, olanzapine, and risperidone. Typical antipsychotics may also produce a small increased risk of death, and more severe extrapyramidal effects and hypotension than the atypicals. Antipsychotic treatment in AD patients should rarely be continued beyond 12 weeks.[13]-[15]
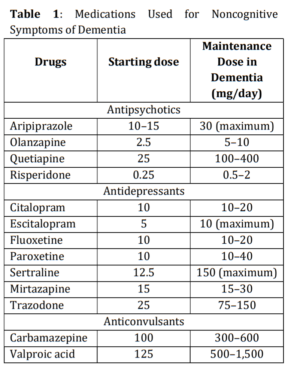
Depression and dementia share many symptoms, and the diagnosis of depression can be difficult, especially later in the course of AD. A selective serotonin reuptake inhibitor (SSRI) is usually given to depressed patients with AD, and the best evidence is for sertraline and citalopram. Tricyclic antidepressants are usually avoided. [16]-[19]
Use of benzodiazepines is not advised except on an “as needed” basis for infrequent episodes of agitation. Carbamazepine, valproic acid, and gabapentin may be alternatives, but evidence is conflicting.[15],[20]

At baseline interview both patient and caregiver, identify target symptoms; define therapeutic goals; and document cognitive status, physical status, functional performance, mood, thought processes, and behavior. The Mini Mental State Examination for cognition, Physical Self-Maintenance Scale for activities of daily living and Neuropsychiatric Inventory Questionnaire for assessment of behavioral disturbances should be used to quantify changes in symptoms and functioning. Observe the patient carefully for potential side effects. The specific side effects to be monitored and the method and frequency of monitoring should be documented. Assess for drug effectiveness, side effects, adherence to regimen, and need for dosage adjustment or change in treatment at least monthly. Several months to 1 year of treatment may be required to determine whether therapy is beneficial. [21]-[23]
References
- 1.Robert PH, Verhey FR, Byrne EJ, et al. Grouping for behavioral and psychological symptoms in dementia: clinical and biological aspects. Consensus paper of the European Alzheimer disease consortium. European Psychiatry. 2005;20:490–496. [Google Scholar] [PubMed]
- 2.Cummings JL, Masterman DL. Assessment of treatment-associated changes in behavior and cholinergic therapy of neuropsychiatric symptoms in Alzheimer’s disease. J Clin Psychiatry. 1998 59suppl 13. 23–30. [Google Scholar] [PubMed]
- 3.Lyketsos C, Steinberg M, and Tschanz JT. et al. Mental and behavioral disturbances in dementia: findings from the Cache County Study on Memory in Aging. Am J Psychiatry. 2000 157:708–714. [Google Scholar] [PubMed]
- 4.Deimling GT, Bass DM.. Symptoms of mental impairment among elderly adults and their effects on caregivers. J Gerontol. 1986;41:778–784. [Google Scholar] [PubMed]
- 5.Rabins PV, Mace NL, Lucas MJ.. The impact of dementia on the family. JAMA. 1982;248:333– 335. [Google Scholar] [PubMed]
- 6.Steele C, Rovner B, and Chase GA. et al. Psychiatric symptoms and nursing home placement of patients with Alzheimer’s disease. Am J Psychiatry. 1990 147:1049– 1051. [Google Scholar] [PubMed]
- 7.Cohen-Mansfield J. Assessment of disruptive behavior/agitation in the elderly: function, methods and difficulties. J Geriatr Psychiatry Neurol. 1995 8suppl 1. 52–60. [Google Scholar] [PubMed]
- 8.Gibson S. A personal experience of successful doll therapy. The Journal of Dementia Care. 2005;13:22. [Google Scholar] [PubMed]
- 9.Gillies BA. A memory like clockwork: accounts of living through dementia. Aging and Mental Health. 2000;4:366–374. [Google Scholar] [PubMed]
- 10.Pulsford D, Rushforth D, Connor I. Woodlands therapy: an ethnographic analysis of a smallgroup therapeutic activity for people with moderate or severe dementia. Journal of Advanced Nursing. 2000;32:650–657. [Google Scholar] [PubMed]
- 11.Lam B, Hollingdrake E, Kennedy JL, Black SE, Masellis M. Cholinesterase inhibitors in Alzheimer’s disease and Lewy body spectrum disorders: the emerging pharmacogenetic story. Human Genomics. 2009;4(2):91-106. [Google Scholar] [PubMed]
- 12.Muayqil T, Camicioli R. Systematic Review and Meta-Analysis of Combination Therapy with Cholinesterase Inhibitors and Memantine in Alzheimer’s Disease and Other Dementias. Dementia and Geriatric Cognitive Disorders EXTRA. 2012;2(1):546-572. [Google Scholar] [PubMed]
- 13.Mohamed S, Rosenheck R, Lyketsos CG, Kaczyinski R, Sultzer D, Schneider LS. Effect of Second Generation Antipsychotics on Caregiver Burden in Alzheimer Disease. The Journal of clinical psychiatry. [Google Scholar] [PubMed]
- 14.Madhusoodanan S, Shah P. Management of psychosis in patients with Alzheimer’s disease: focus on aripiprazole. Clinical Interventions in Aging. 2008;3(3):491-501. [Google Scholar] [PubMed]
- 15.Stevenson DG, Decker SL, Dwyer LL, et al. Antipsychotic and Benzodiazepine Use Among Nursing Home Residents: Findings From the 2004 National Nursing Home Survey. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2010;18(12):1078-1092. [Google Scholar] [PubMed]
- 16.Peters ME, Vaidya V, Drye LT, et al. Citalopram for the Treatment of Agitation in Alzheimer Dementia: Genetic Influences. Journal of geriatric psychiatry and neurology.2016;29(2):59-64. [Google Scholar] [PubMed]
- 17.Zhu CW, Livote EE, Kahle-Wrobleski K, et al. Utilization of Antihypertensives, Antidepressants, Antipsychotics, and Hormones in Alzheimer’s Disease. Alzheimer disease and associated disorders. 2011;25(2):144-148. [Google Scholar] [PubMed]
- 18.Cipriani A, Purgato M, Furukawa TA, et al. Citalopram versus other anti-depressive agents for depression. The Cochrane database of systematic reviews.2012;7:CD006534. [Google Scholar] [PubMed]
- 19.Geerlings MI, Brickman AM, Schupf N, et al. Depressive symptoms, antidepressant use, and brain volumes on MRI in a populationbased cohort of old persons without dementia. Journal of Alzheimer’s Disease.2012;30(1):75-82. [Google Scholar] [PubMed]
- 20.Venkataramani V, Rossner C, Iffland L, et al. Histone Deacetylase Inhibitor Valproic Acid Inhibits Cancer Cell Proliferation via Downregulation of the Alzheimer Amyloid Precursor Protein. The Journal of Biological Chemistry. 2010;285(14):10678-10689. [Google Scholar] [PubMed]
- 21.Borson S, Frank L, Bayley PJ, et al. Improving dementia care: The role of screening and detection of cognitive impairment. Alzheimer’s & dementia : the journal of the Alzheimer’s Association. 2013;9(2):151-159. [Google Scholar] [PubMed]
- 22.Hyman BT, Phelps CH, Beach TG, et al. National Institute on Aging–Alzheimer’s Association guidelines for the neuropathologic assessment of Alzheimer’s disease. Alzheimer’s & dementia : the journal of the Alzheimer’s Association. 2012;8(1):113. [Google Scholar] [PubMed]
- 23.Chapman KR, Bing-Canar H, Alosco ML, et al. Mini Mental State Examination and Logical Memory scores for entry into Alzheimer’s disease trials. Alzheimer’s Research & Therapy. 2016;8:9 [Google Scholar] [PubMed]