Department of, Biochemistry, Faculty of Medicine, University of Benghazi, Libya.
Email: nasibnm.2014@gmail.com
Background: Hyperbilirubinemia refers to the yellow coloration of the skin and the sclera of newborn babies that result from the accumulation of bilirubin in the skin and mucous membranes. Newborns with jaundice need to be monitored because bilirubin is potentially toxic to the central nervous system
Aim of the study: To determine the relation of erythrocytic glutathione with hyperbilirubinemia in newborns
Methods: We studied 45 Libyan full-term newborns (23 male and 22 female) with neonatal hyperbilirubinemia aged from day one to day four born in AlJomhoriya hospital in Benghazi.We excluded each case with pathological jaundice that needs treatment by phototherapy or blood exchange. All investigations concerning this research carried out on each newborn every 24 hours in a period of four days as follow: day 1 up to day 4, day 2 up to day 5, day 3 up to day 6, day 4 up to day 7. We analyzed the total serum bilirubin (TSB) and the level of reduced glutathione (GSH) in red blood cells directly on fresh blood.
Conclusion: Our results show no significant variations in the mean level of erythrocytic glutathione in the jaundiced full-term newborns compared to the control group in the first week of life.
Keywords: Infants, Glutathione, Newborns, Jaundice, Hyperbilirubinemia
Neonatal jaundice refers to the yellow coloration of the skin and the sclera (whites of the eyes) of newborn babies that result from the accumulation of bilirubin in the skin and mucous membranes. This is associated with a raised level of bilirubin in the circulation, a condition known as hyperbilirubinemia. [1] Some 60% of normal newbornsbecome clinically jaundiced sometime during the 1st week of life. Unconjugated (indirect) hyperbilirubinemia occurs as a result of excessive bilirubin formation and because the neonatal liver cannot clear bilirubin rapidly enough from the blood.[2],[3]
Newborns with jaundice need to be monitored because bilirubin is potentially toxic to the central nervous system. Sufficiently elevated levels of bilirubin can lead to bilirubin encephalopathy and subsequently kernicterus, with devastating, permanent neuro-developmental handicaps.[4] Bilirubin is normally cleared from the body by hepatic conjugation with glucuronic acid and elimination in bile in the form of bilirubin glucuronides. Neonatal jaundice stems from a transient deficiency of conjugation (exacerbated in preterm infants) combined with increased turnover of red cells. Pathologic conditions that can increase bilirubin production include isoimmunization, heritable hemolytic disorders,and extravasated blood.[5]
Reduced glutathione (GSH) is a tripeptide thiol (γglutamyl-cysteinyl-glycine), present in most cells of the human body and commonly in erythrocytes that are known to have numerous biological functions. This thiol group of reduced glutathione plays a prominent role in detoxification and antioxidation of exogenous and endogenous compounds, as well as maintaining the intracellular redox status. Hyperbilirubinemia is a common and, in most cases, benign problem in neonates. Nonetheless, untreated, severe unconjugated hyperbilirubinemia is potentially neurotoxic in infants at a certain concentration and under various conditions. Red blood cells with a lowered level of reduced GSH are more susceptible to hemolysis due to the accumulation of H2O2 and other oxidants that decrease the life span of erythrocytes. Many references emphasize that decreasing levels of reduced (GSH) erythrocytes lead to hemolytic anemia and maybe also Jaundice in newborns. In this study, we aimed to identify the relation of glutathione with hyperbilirubinemia.
We studied 45 Libyan full-term newborns (23 male and 22 female) with neonatal hyperbilirubinemia aged from day one to day four born in Al-Jomhoriya hospital in Benghazi in the period from 1st June 2007 to 30th September 2007. The age-matched subjects were divided into two main groups: The first one, (15) subjects with bilirubin level does not exceed 5.5 mg/dl and clinically not jaundiced chosen as a control group. The second one, (30) subjects chosen as tests with clinical jaundice and bilirubin level between 6 mg/dl and 16 mg/dl. This group was subdivided into two groups as follow:
1. Fifteen newborns without ABO blood group incompatibility named (Non-ABO group).
2. Fifteen newborns with ABO blood group incompatibility named (ABO group). We excluded each case with pathological jaundice that needs treatment by phototherapy or blood exchange. We analyzed the total serum bilirubin and the level of reduced glutathione in RBC and directly on fresh blood.
Test principle[6]:
Manual Colorimetric method (Beutler, E, Duron O. and, Kelly B. Improved method for the determination of blood glutathione. Journal of laboratory and clinical medicine. 61: 882, 1963).This method is based on the reduction of 5, 5′
dithiobis (2-nitrobenzoic acid), (Elman’s reagent,DNTB) with glutathione (GSH) to produce a yellow compound. The color which develops is fairly stable for about 10 min and the reaction is little affected by variation in temperature. The reduced chromogen is directly proportional to GSH concentration and its absorbance can be measured at 405 nm. Sample: Fresh blood in EDTA tube.
Reagents:
Reagent 1: precipitating reagent, trichloroacetic acid (TCA) 500mmol/L
Reagent 2: Buffer (Phosphate solution) 100 mmo/L
Reagent 3: 5,5′ dithiobis (2-nitrobenzoic acid) (DNTB) 1.0 mmo/L
Sample Preparation: Plasma and erythrocytes lysate The venous blood was collected using an anticoagulant of EDTA tube. The blood then was centrifuged at 700 – 1000 ҳ g for 10 minutes at 4 °C. The top yellow plasma layer was Pipet off without disturbing the white buffy layer. Store plasma on ice until assaying GSH or freeze at -80 °C. The plasma sample will be stable for at least one month. The white buffy layer was removed and discarded. Lyse the erythrocytes (red blood cells) in 4 times its volume of ice-cold HPLC grade water. The lysate was centrifuged at 4000 ҳ g for 15 minutes at 4 °C. The supernatant was collected for assaying and store on ice. If no assaying on the same day, freeze at -80°C. The sample will be stable for at least one month.
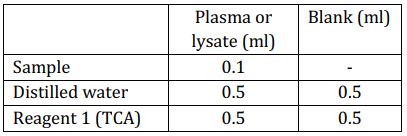
Mix well, allow standing for 5 minutes at room temperature. Centrifuge at 3000 rpm for 15 minutes, and then take the following aliquots
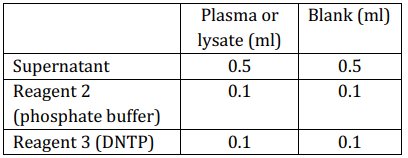
Mix well and measure the absorbance after 5-10
minutes at 405 nm of the sample (A sample) against the blank.
Calculation:
GSH concentration in red blood cells or plasma = A
sample x 66.66 mg/dl
= A sample x 2.22 mmol/L
Expected values in adult:
69 ± 11 mg/dl packed red cell. 24-37 mg/dl in
whole blood.
The Cobas Integra Bilirubin Total (BIL-T) cassette contains an in vitro diagnostic reagent system intended for use on Cobas Integra systems for the quantitative determination of the total bilirubin concentration in serum (test BIL-T, 0-048).
Test Principle: Diazo Method[7]
Since the absorbance maximum for azobilirubin is pH-dependent, and oxalic acid/sulfanilic acid buffer system is used to maintain the pH of the reaction. The color intensity is proportional to the concentration of total bilirubin in the sample and is determined by monitoring the increase in the absorbance at 552 nm. Reagents-working solutions: (ready for use)
R1: Sulfanilic acid in vial A (liquid)
R2: Nitrite in vial B (liquid).
Calculation:
Cobas Integra analyzers automatically calculate the analyte concentration of each sample.
Conversion factor: µmol x 0.0585= mg/dl
Expected values:
Adults and children: < 1.0 mg / dl
Neonate’s full- term (3 to 5 days): < 12.0 mg /dl
Neonate’s full- term (2 days): < 7.0 mg /dl
Neonate’s full- term (1 days): < 6.0 mg /dl
Table 1and figure 1 illustrates the mean levels of RBC-GSH (mg/dl) in different groups according to age in the first week of life. It was clear that there was no significant difference in the mean level of RBC-GSH between jaundiced groups and the control. Moreover, there was no significant difference in the RBC-GSH at different days in the first week of life in the three groups.
In the next Table (2) and figure (2) show the total serum bilirubin (mg/dl) in different groups according to the baby’s ages in the first week of life. It was clear that the levels of bilirubin in both control and Non-ABO groups increased gradually every day and reached the peak at day 5 then decreased gradually, but in the ABO group, there was a gradual increase in TSB every day with no tendency to decrease.
Table 2 also clarifies the criteria of the study groups according to bilirubin concentration as follow:
1. In the first of24 hours, the highest mean bilirubin level was present in the ABO group (4.72 mg/dl); therefore, the symptoms of ABO jaundice appeared earlier than Non-ABO group which had TSB (3.82 mg/dl) lesser than ABO.
2.On day 2 the level of bilirubin in ABO and NonABO groups reached the level that clinical physiological jaundice symptoms appear (> 6 mg/dl).

P is significant at level ≤ 0.05
Table 1: RBC-GSH (mg/dl) in different groups according to age in the first week of life

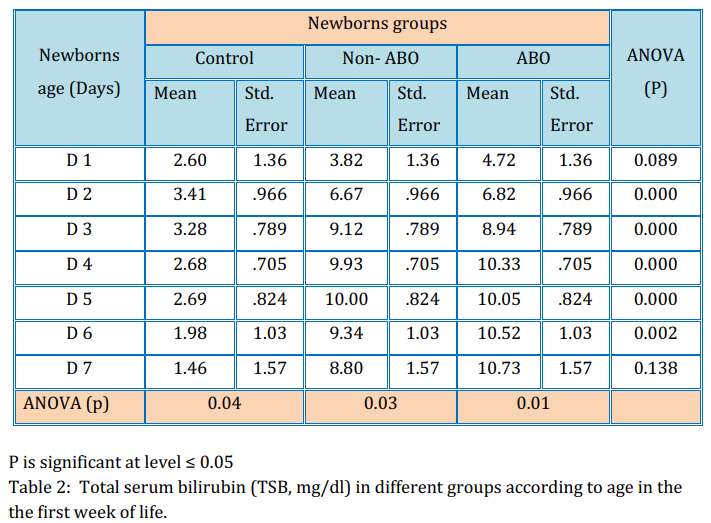
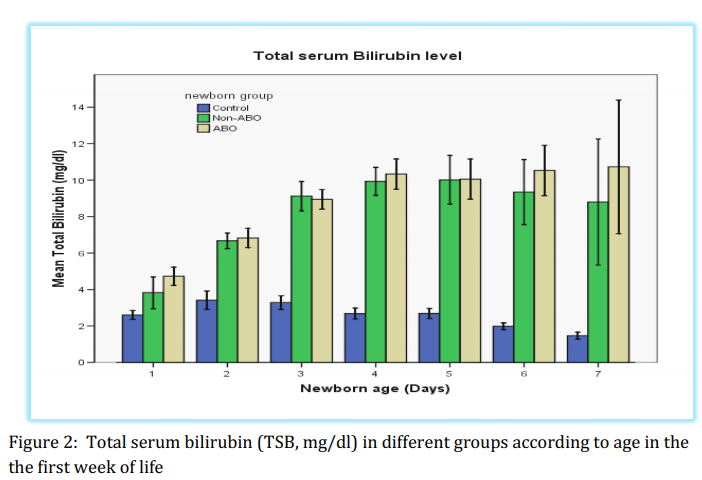
3. In both jaundiced groups (ABO & Non-ABO) the mean level of TSB did not reach the pathological levels that need treatment (Max = 10.7 mg/dl).
4. In the control group the mean levels of TSB were under 5.5 mg/dl, there were no symptoms of clinical jaundice appearing in this group.
In this prospective study, we aimed to investigate the variation between erythrocytic GSH levels in full-term jaundiced newborns and control group and this could give us an explanation that why some newborns have neonatal jaundice but the others not.
The hypothesis of this study suggests that the accelerated breakdown of erythrocytes which is one of the factors responsible for neonatal hyperbilirubinemia may be due to instability of red cell membrane that might be possible as a result of the lowered level of GSH in RBC which has a basic role in the protection of cell membrane fromoxidants and hence enhance the integrity of cell membrane of RBC
Reduced GSH level in RBC: The result of the study showed that the distribution of the mean level of reduced GSH in RBC in all three different groups according to the ages in the first week of the life of newborns (Table 1), that would have answered the first aim in this present study. It was clear by using the ANOVA test between all three groups that there were no significant variations in the GSH level between both jaundiced groups (ABO & Non-ABO) compared to the control group (table 1).
Besides, it has been found from our results that there was no significant difference in the mean level of reduced GSH between days 1 up to day 7 within all three groups (figure 1). Our study findings are in the line with the previously
published study.[8]
By comparing the changes in the mean levels of erythrocyte GSH (Table 1) with the mean levels of TSB (table & figure 2) within both jaundiced groups (Non-ABO & ABO), it is clear that the erythrocyte GSH levels in all 7 days with both groups were mostly stable while the TSB levels in both groups were unstable and there was a significant increase in TSB with increase days.
Our study findings are in the line with the previously published report who studied the RBCGSH in the twelve newborns between day 2 and day 5 with physiological jaundice and reported that all the twelve cases except one case showed normal GSH level.[9],[10]
Therefore, those results showed the first indication that the reduced GSH possibly has no significant
role in the occurrence of hyperbilirubinemia in fullterm newborns in the first week of life.
There were no significant variations in the mean levels of erythrocyte GSH in both jaundiced groups (Non-ABO & ABO) compared to the control group in the first week of the life of full-term newborns and the erythrocyte GSH has no significant role in the induction of neonatal hyperbilirubinemia in fullterm newborns in the first week of life.
Much work should be done in the future to measure other parameters that might be participating in the pathogenesis of neonatal hyperbilirubinemia to know why some full-term newborns are affected clinically with neonatal jaundice but others do not affect in the first week of life.
References
- 1.Welsh A. London: Published by the Royal College of Obstetricians and Gynaecologists; 2010. Neonatal jaundice. [Google Scholar] [PubMed]
- 2.Sies H. Oxidative stress: From basic research to clinical application. Am J Med. 1991;91:31S–8S. [Google Scholar] [PubMed]
- 3.Johnson J. Glenview, IL, United States of America: Mead Johnson and Company; 1993. Jaundice and your baby; pp. 1–4. [Google Scholar] [PubMed]
- 4.Melton K, Akinbi HT. Neonatal jaundice. Strategies to reduce bilirubin-induced complications. Postgrad Med. 1999;106:167– 8. 71 [Google Scholar] [PubMed]
- 5.Britton JR, Britton HL, Beebe SA. Early discharge of the term newborn: A continued dilemma. Pediatrics. 1994;94:291–5. [Google Scholar] [PubMed]
- 6.OWENS CW, BELCHER RV. A COLORIMETRIC MICRO-METHOD FOR THE DETERMINATION OF GLUTATHIONE. Biochem J. 1965;94(3):705- 711. [Google Scholar] [PubMed]
- 7.Engle WD, Jackson GL, Sendelbach D, Manning D, Frawley WH. Assessment of a transcutaneous device in the evaluation of neonatal hyperbilirubinemia in a primarily Hispanic population. Pediatrics. 2002;110:61-67. [Google Scholar] [PubMed]
- 8.Pastore A, Piemonte F, Locatelli M, Lo Russo A, Gaeta LM, Tozzi G, Federici G. Determination of blood total, reduced, and oxidized glutathione in pediatric subjects. Clin Chem. 2001 Aug;47(8):1467-9. . [Google Scholar] [PubMed]
- 9.Pati HP, Singh M, Paul VK, Gupta RK, Saraya AK. Cord blood red-cell enzymes and reduced glutathione in Indian neonates, normal and with pathologic jaundice. J Trop Med Hyg. 1990 Aug;93(4):290-4. [Google Scholar] [PubMed]
- 10.Casado A, Casado C, López-Fernández E, de la Torre R. Enzyme deficiencies in neonates with jaundice. Panminerva Med. 1995 Dec;37(4):175-7. [Google Scholar] [PubMed]

