*Corresponding author at: Department of Bioengineering, Integral University, Lucknow-226026, Uttar Pradesh, India. mkakhan@iul@ac.in https://orcid.org/0000-0002-8004-1448 https://doi.org/10.37881/1.638
With the transforming world, awareness of lifestyle-based variation is necessary. The availability of the locally available network and smart devices like wearable health devices (WHDs) based on artificial intelligence (AI) technology prompted us to learn about the disease, its causes, spreads, and precautions. Socioeconomic, environmental and behavioural factors, international travel and migration foster and increase the spread of communicable diseases. Vaccine-preventable, foodborne, zoonotic, healthcare-related and communicable diseases pose significant threats to human health and may sometimes threaten international health security. On the other hand, non-communicable diseases, also known as chronic diseases, are more prolonged. It could be the cause of different factors like genetic, environmental, behavioural or physiological disturbances. Smart wearables help to keep these diseases in check through different sensors installed in them. They can check for the difference in body function, but they can also help the needy consult the physician or practitioner. The data collected from these devices can also check the current health status when compiled with data collected practically. Organizations viz., World Health Organization (WHO), Food and Drug Administration (FDA) work collaboratively, leading global efforts to expand health coverage. WHO keeps the nation safe through connecting its people on the health and awareness interactive platforms, and FDA promotes public health through supervision and control, defending its role in human health and services.
KeywordsCommunicable disease, Non- communicable disease, AI-based wearable health devices. WHO, IDF, FDA,
Technology is changing the world. Artificial Intelligence (AI) is domineering the world and helping in daily life health issues through AI-based health care gadgets. AI proved itself as a priceless asset to humankind. Almost every person, irrespective of their age and gender, uses these AI-based gadgets in one way or another. The AI-based wearable health devices (WHDs) can track their health status in both fitness level and self-health tracking at the medical level and make them known about potential earlier diagnostics of diseases and guidance for treatment by providing their data to experienced physicians/clinicians.[1]-[4] The small size and efficiency in the performance of wearable health devices like smartwatches empower the worldwide change in the health monitoring approach. The WHDs with recent developments can track/perform electrocardiograms, heart rate, blood pressure, body temperature,blood oxygen saturation, blood glucose, and skin perspiration. A global review showed that these devices decreased the accidental deaths because of cardiovascular and blood pressure abnormalities in the people wearing these health devices.[5]-[7] These devices, by keeping the record vitals, can also help individuals who feel discomfort going to hospitals or clinics for regular check-ups, and the meantime can also save their time. WHDs were introduced in late 1990 to make individuals manage their health by interacting with care providers. This program was supported as a ‘patient empowerment’ program. These devices create a globally accessible platform between multiple science domains such as biomedical technologies, micro and nanotechnologies, material engineering, information, and communication technologies.[2],[4],[8]-[12] According to Statista, wearable devices currently making worldwide revenue of 59.41 billion dollars and can reach about 73.27 billion dollars in the year 2022. The annual revenue shows a regular increase from 2016. Smartwatches can alert friends, family, and healthcare workers about conditions like seizure and tremors, which needs quick and effective treatment.[13] The diseases are categorized into two broad categories: Communicable diseases and noncommunicable diseases. Communicable diseases are agent-specific and vector-borne. The host of communicable diseases needs one or more material mediums to propagate, like air, water, food or the host body. The communicable diseases can be climate-sensitive vector-borne, like malaria, dengue, schistosomiasis, Chagas disease and African trypanosomiasis.[14],[15] Not only they can cause death, but they can also cause significant debilitation and suffering. Communicable diseases are more common in the tropical climates of developing countries. Socio-economic coverage and health services in the area also contribute to the reasons. The mortality rate of communicable diseases is 300 times more in developing nations due to these factors. Communicable diseases can disturb the overall health system, tourism sector, country development rate, and socio-economic status. It is correlated with poverty, and the comparatively unprotected population has poorer environmental and social conditions.[16]-[18] The WHO reveals the importance of vector-borne diseases states that previously relatively stable geographical distributions are deforestation, population movement, rapid unplanned urbanization, and phenomenal international travel and trade increments. The observational evidence strengthens the effects of meteorological factors from seasonal and interannual patterns of diseases in specific locations. There were about 207 million cases and [6],[27],000 deaths attributable to malaria in 2012. The recent pandemic, which left the victims disturbed, was caused by one of the most recent and potentially communicable diseases, i.e., Coronavirus disease (COVID-19).[19],[20] Non-communicable diseases (NCDs) fall in the category of chronic disease. They tend to be of long duration and result from genetic, physiological, environmental, and behavioural factors. Main NCDs are cardiovascular diseases, cancers, chronic respiratory disease (chronic obstructive pulmonary disease and asthma), and diabetes, mostly seen within the average income countries.[15],[21]-[23] NCDs kill about 41 million people each year, equivalent to 71% of all deaths globally. Each year, more than 15 million people die from NCDs between the ages of 30 and 69 years; 85% of these premature deaths occur in low- and middle-income countries. 80% of all NCDs premature deaths are cardiovascular disease (17.9 million deaths), cancers (9.3 million deaths), respiratory disease (4.1 million deaths) and diabetes (1.5 million deaths).[24],[25] These diseases are driven by forces like globalization, unplanned urbanization of unhealthy lifestyles and population ageing. The sedentary lifestyle can be the reason for high blood pressure, hyperglycaemia, hyperlipidaemia, and obesity. In terms of attributed deaths, the leading metabolic risk factor globally is elevated blood pressure followed by overweight and obesity and hyperglycaemia. NCDs compromise progress towards the 2030 agenda for sustainable development, which incorporates decreasing unexpected losses from NCDs by 33%. Poverty is strongly associated with NCDs. The exponential increase in NCDs impedes poverty reduction initiatives in low-income countries, particularly by increasing household costs associated with health care. The WHO and the FDA keep the world in check and help control the diseases spread through supervision, control, and awareness. The WHO Academy brings the latest innovations in adult learning to global health. Using the latest technologies will enable all learners to tailor their learning experiences to meet their own needs.[26]-[28] The FDA helps by increasing the availability of generic drugs to make the treatment more affordable and increase access for more patients.[29]-[32] FDA, while working with federal agencies like the drug enforcement administration, customs and border protection, and consumer product safety commission of United States Department of Agriculture (USDA), regulates almost every facet of the prescription drug, including testing, manufacture, labelling, and advertising. The disease supervision and check are currently volunteered through gadgets like smart health wearables and online interactive platforms. These gadgets and interactive platforms help individuals to keep their health or disease in control through self-check.
Wearable technology works on the principle of collecting data by taking snapshots through motion sensors. The data is collected at different body conditions like static and dynamic. The data is then transferred to the connected system, where custom applications analyse it.[2],[4],[9],[33],[34] As the consumer electronics industry invests hugely in health wearables, a massive explosion in demand is seen in devices like Apple, Samsung, and Huawei. In contrast, some devices also lost their momentum and disappeared from the market as they kept up with the advancement of AI-based health technology’s efficiency (Figure 1). The global health wearable devices reached a market worth of USD29.76 billion in 2019 and continuously projected a target of USD 195.57 billion by 2027, exhibiting a Compound Annual Growth Rtae (CAGR) of 26.4% during the forecast period. With reduced size and comfort in wearables and suitable sensors, they provide continuous data about vitals and environmental variables.[13],[35],[36] Different gadgets are evading the market based on their availability, efficiency of work and sensors present. Apple is ruling the market with their gadgets, especially smart wearables (Figure 2).
Figure 1: Worldwide shipments of smart wearables by Statista

Figure 2: Device wise market share in 2021 (2nd quarter) by Statista

The applications of intelligent health gadgets vary with person and demand. Applications include simple call making, listening to music or daily health track of organs functioning like heart rate, blood pressure according to the sensor. They also calculate the calories burnt during a workout and provide users with health-based exercise standards (Figure 3).
Figure 3: Applications of smart health wearable.

Wrist bands equipped with sensors help track users’ physical activity and heart rate. The sleek design of these watches fascinated the users, along with their tracking capacity. An android app transfers the data from watches with fitness trackers to smartphones, which is then stored in the warehouse.[13],[37],[38] These trackers are equipped with a 3-axis accelerometer and sometimes with altimeter, gyroscope, and optical sensors. Different devices are equipped with different features according to their work. Accelerometer track movements and gyroscope the orientation and rotation altimeter measure the altitude of the mountains climbed or flights managed. They can calculate the duration, frequency, intensity, acceleration as well as patterns of movement. Fitness trackers like Fitbit also provide warehouse REST API access to third-party developers through specific permissions like per minute heart rate.[39]-[42]
Smartwatches are smart wrist wearables with integrated features of digital watches and smartphones. The idea was to save the person from awkward moments during meetings or other sensitive occasions and keep them updated with all the calls and work notifications. Smartwatches offer touchscreen access to apps (media, calculator, GPS, battery life), receiving and making calls, getting all types of phone’s notifications, and recording heart rate and other vital signs.[35],[43]-[47] Companies like Apple offer smartwatches for daily use. Companies like Garmin Fenix offer smartwatches for specific/sensitive purposes, which are more optimised and rugged with trackers and sensors used to support back-country expeditions and Suunto smartwatches for scuba diving. According to Statista, 115 million smartwatches global shipment was made in 2020 with expected to rise to 258 million global shipments by 2025.[48],[49]
Compared to everyday smartwatches, electrocardiograms done by ECG specific smartwatches are tremendously sensitive and effective in detecting any issue that may arise. An ECG can detect various problems like coronary heart disease, cardiomyopathy and even sometimes heart attack. It was designed by the idea of taking an ECG spot reading any time and thus making it a powerful health tool for human welfare. Companies like Apple, Samsung, and Withing provides a good series of ECG supporting smartwatches.
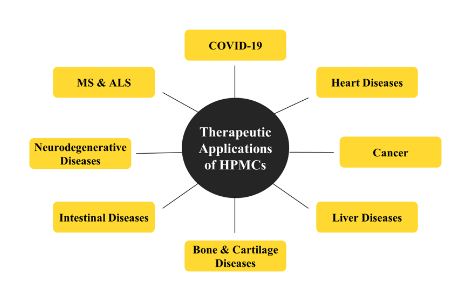
Figure 1: Therapeutic applications of human placenta-derived mesenchymal stem cells against various diseases
watch actives use biological data to calculate pulse transit time to approximate the blood pressure. The pulse transit time is a measurement of the time taken by a heart pulse wave to travel throughout the two ends along an artery. It uses an oscillometer monitoring device to examine blood pressure. These monitors are moving with a high success rate as most of the todays’ population is experiencing hypertension leading to high chances of haemorrhage, kidney failure and cardiac arrest. The recent technology is still not a good match for the accuracy of the traditional home monitors, but with the development, this may overtake the old traditional monitors. To ensure accuracy, a standard is set with a ratio of systolic to diastolic blood pressure at 120/80 mmHg. To the app’s accuracy, users are asked to measure their blood pressure using a phone or watch several times a day and answer questions related to their daily routines; then, these data are stored and analysed accordingly.
Sensors integrated within clothing, like smart-shirts and smartwatches, are the basis of wearable biosensors. It uses a self-adhesive patch facility. The information is then sent to the healthcare providers. It is also used in the military to supervise soldiers or people during hazardous operations and overcrowded emergency departments with hazardous elements. It can also sense symptoms like hypertension and heart failure. Patients needing remote monitoring, trainees during an athletic workout, professionals during heavy vehicle driving uses these biosensors for tracking.[37],[48],[50]-[56]
Components like hardware (viz., devices and sensors) and software (viz., data collection and analysis) are integrated to form the proper functioning unit of the wearable (Figure 4).
Figure 4: Components necessary for the working of smart health wearable.

Portable skulls made up of diverse material are chosen by the brands according to their model type and expected function of the device. The right choice of material is necessary for the permanency of the wearable and its aesthetics. Silicone rubber watches are soft and rubbery in texture.[57]-[59] The screen is among the essential elements of intelligent wearables as these are needed for input and output displays. Divided into two parts: touch panel and intelligent display. OLED (AMOLED and PMOLED), E-ink, Traditional LCD and sharp memory LCD are screen types used in smartwatches. The battery is another crucial part of the functioning of smartwatches. Lithium Polymer and Li-ion batteries provide prolonged battery life.[60]-[65] Technology is developing further with solar supported and chargeable (wired and wireless) smartwatches.
The operating system (OS) embedded in the intelligent wearables allows third-party users to install and access data. This domain is essential as it allows data collection at significant levels for further research and development.[66] Different companies are providing their own Oss and software platforms like Flyme OS by Meizu (China), watch OS by apple watch (America), Wear OS by Google Inc. (America), Tizen, an opensource software under Linux foundation by Samsung Electronics, Asteroid OS an opensource software, Ubuntu Touch by Ubuntu community and Canonical UK Ltd (funded by South Africa), Infini Time by pine64 for Pine Time Smartwatches.[67],[68] According to a report by Mordor Intelligence, the smartwatch market is the fastest-growing market in the Asia Pacific, with North America having the largest market share. The expected growth rate of (CAGR) is 14.5% over the forecast period from 2021- 2026.
Different sensors for different functions are installed in intelligent wearables.[40] An ambient light sensor helps to tweak the brightness as per the surrounding light intensity. Another feature of ambient light sensors is to help save battery. The accelerometer detects any movements in the body, its orientation and gravity action and speed of movements. Gyroscope and motion detection also determine whether the person is actually running or simply jogging by measuring angular velocity during the workout. Optical heart sensors sense the blood flow inside the arteries and sense the light reflected, further detected as a heartbeat per minute.[9],[46],[53],[69]-[72] Saturated peripheral Oxygen (SpO2 ) monitor sensor senses the relative reflection of red and infrared light from the blood, returned through veins and calculates the SpO2 value. SpO2 value is estimated through the oxygen level present in the blood. The darker the blood more will be the more oxygen level in the blood. Bio-impedance sensors are used to measure respiratory rate. This sensor also senses when the person sleeps and turns off the display screen, which helps save battery life.[73],[76] Compass gives the device a sense of direction and allows the user to use the map. ECG sensors are a new type of sensor used to detect electrical impulses. The sensors detect the electrical impulse sent by the heart with the help of electrodes. Gesture sensors are sensitive to wrist motions. They accept wrist movements as the commands given by the user, like when it senses the hand movement in a circle, activates the stopwatch. The UV sensors sense sunlight. Magnetometer to sense and determine the exact coordinates of location with the help of GPS. The skin temperature sensor detects abnormal conditions like fever and the start of the menstrual cycle by detecting the change in body temperature.
The data is collected with the help of sensors already installed in the smart wearables. This data is then stored in the connected smartphones, computers, servers, or cloud services. Vendors or producers maintain this data and check for the ethical transfer while providing the authorized third party to perform analytics.[7],[46],[49],[77]-[81] Acts like Electronic Communications and Privacy Act (ECPA), Children’s Online Privacy Act (COPA), and Federal Trade Commission (FTC) enforce laws for ethical data collection.
The data can be transferred in various ways to third parties, analytics, and warehouse servers. Data transfer through different devices like smartwatches, cloud servers and computers. Apple stores data in apps, SDK, Cloud, and Apple health warehouse and provides analytic services. The Health kit (Software Development Kit (SDK)) of Apple can be accessed by iWatch, iPhone, iPad through their app. Google also provides SDK services along with REpresentational State Transfer (REST) Application Programming Interface (API) for third-party systems along with cloud services and warehouses. REST is a software architectural style that was created to guide the design and development of the architecture for the World Wide Web. REST defines a set of constraints for how the architecture of an Internet-scale distributed hypermedia system, such as the Web, should behave Google provides its devices with the best sensors, so the data collected is equal to accurate, giving noticeable results. Another app like S-Health used by smartphones gains access to collected data through the proprietary warehouse. Fitbit’s only provides REST API for third-party. Microsoft health provides both SDK and REST API.
Data is accessed directly or indirectly from the registered warehouse or directly from a wearable in various ways (Figure 5). When accessed from the warehouse, no processing time is needed before.[63],[66],[82]-[85]
Figure 5: Diagrammatic representation of data access methods in WHDs.

Direct access from the wearable approach is quite advanced as a direct gateway is made between the wearable and a third party. Permanent network access is required to fulfil this demand. Samsung Gear S2 uses this technology and needs further improvement as the current power demand is too high (Figure 6a). Indirect access from the wearable is through an app in the availability of internet access. The data is stored in the app irrespective of the availability of an internet connection (Figure 6b). Direct access from the warehouse is obtained through REST API. The intermediate wearable or computer system acts as a gateway towards the server using Bluetooth (Figure 6c). SDK supports indirect access from the warehouse. The wearable sends the data from the device to SDK through REST API (Figure 6d).

Figure 6: Diagrammatic representation of Data access in WHDs: a) direct, b) indirect, c) direct access from warehouse, d) indirect access from warehouse
After receiving data from wearable either directly or indirectly, the next step is data integration and analysis based on the requirement. Data is arranged on the basis required parameter like heart rate, sleep record, weight, calories, and daily activities.[63],[77],[79],[82],[86],[87] The analysis is made based on different data models, data names, temporal discrepancies, or counters. Data models like JSON or XML are used to track different segments like sleep time, sleeping state and awake time. Each data model has unique ids like learners’ id strings and long integers. An algorithm like Kstar helps in tracking the persons’ sleep through indicators like Pittsburgh Sleep Quality Index. The training data is tracked for a period of a minimum of 30 days. Factors like skin temperature and heart rate are considered.[48],[79],[87]-[89]
Data privacy
The sensitive information gathered by the users’ lifestyle devices concerns many privacy-related issues. The availability/access of data through the internet of things (IoT) significantly activates an innovative learning paradigm in the healthcare sector. A gateway could be formed during data upload in the wearable cloud, leading to attack or data leakage. Technical defects could also lead to data overflow.[80]-[82]
Network
As the innovative wearable works on the digital platform, data storage in the cloud needs unobstructed network availability. Also, all the system elements are joined on the virtual platform via different networks, and the data needs on-time synchronization to give a real-time result. So, any hindrance in the network availability could lead to failure in data collection or successful sync.[51],[90],[91]
Asynchrony
It is also related to the network issue; as with the network outage, the whole system becomes asynchronous. Regular network availability is required to manage this issue. High power consumption protocols could also contribute to asynchrony as the low energy can disrupt the working of the device.[1],[66]
Sustainability
The sustenance of the device for a more extended period is necessary for any device to be considered a success in the invention. The device should be resistant to vigorous movements like jolting, environmental changes, possible physical damage and accidents. Violent body movements could affect the effectiveness of the sensors used, and therefore, the device must filter these disturbances and retain its work sensitivity without any fail.[92]
Availability
With increasing demand and consciousness towards health care activities, a surge in health wearable demand is seen. The middle class and poor population are still unavailable to avail of this facility due to high price, illiteracy, and network issues in rural or underdeveloped areas.[93]-[97]
Convenience and ergonomics
Ease to carry with a defined shape as described by Ferraroa and Canina, 2011. The device must be easy to carry, and the wearer should not feel any discomfort. A device like smart clothing should be loaded with technology that can make it odour-free and fresh throughout. Another point is that the material should not make skin irritations and provide a good framework for the wearable.[4],[12],[59],[80],[98]-[100]
Limited resources
The device’s design plays a significant role in making it portable and handy. Network availability and energy resource constraints the design.[7],[101]
Self-organized online wellness knowledge-transfer interactive platforms, formed between patients and health officers, caregivers, or researchers to develop the health solutions and to motivate and create awareness regarding disease and disease resistance. Online health platforms form an ecology of different and lightly bound communities operating on various digital positional platforms, which broadly evolves around traditional health policy and health care institutions.[102],[103] The wellness platform conducts assessments to educate through webinars, videos, books, audio files, social media, and individualized feedback. The track program participation activity makes engagements through digital platforms like mobiles, provides the tools needed to be healthy, deliver behavioural change campaigns, and create a healthy health culture.[103]-[104] The health assessments made by accessing data from the individual user to conduct health tests are kept entirely confidential. The result is then used to encourage and educate the individuals about their healthy lifestyle and disease resistance. Platforms like IBD relief, OpenWHO, Care Opinion, Patients like Me, Genetic Alliance, Kickstarter, 38 Degrees, Move on, and OpenIDEO helps to create open health interactive platforms.[105] However, this field is still progressing with the latest advances with new health trends and levelling up with their peer-to-peer technology by advancing in therapies, exchanging, and providing reliable information about ‘former experience’, patient-led innovations, and shaping digital technology regularly. These platforms are cheaper, are more publicly available and promote facilitated research with gift economies. The members themselves provide information about their experiences and treatments they took. It helps the patients gather their strength to fight from disease both physically and mentally as the members also share the torments and pains during their bare survival period.[105] OpenWHO was the first WHO platform to host unlimited users during health emergencies; it provides the users/patients with the fastest free way to obtain the latest scientific and operation technologies. It also offers offline downloads, discussion forums, and updates related to health emergencies. The salient features of Online interactive platforms include Confidential health assessments, easily accessible platform, programs to track activity, information about general health awareness, regular behavioural health campaigns with awareness and challenge, create a health-promoting culture, and affordable consultation charges.
With the ongoing trends, it will not be wrong to say that the crowds in the hospital for mere consultations and small tests like blood pressure check-ups will soon lessen with the emergence of technologies like intelligent health gadgets and online interactive platforms. Every day companies are working and coming out with newer and better works and lesser and more affordable price ranges. The global health market is escalating with new and sensitive health-related products. The awareness programs are playing a significant role in educating the world about this change. Due to some reasons, illiteracy, and urban areas with little or no network connectivity are still significant drawbacks to accessing the merits of global health digital platforms.
The author declares that there are no conflicts of interest relevant to this article.
WHO: World Health Organization, FDA: Food and Drug Administration, NCDs: Non-communicable diseases, AI: Artificial Intelligence, WHDs: Wearable Health Devices, SDK: Software Development Kit, REST API: REpresentational State Transfer, IoT: Internet of Things, IDF: International Diabetes Federation, USDA: United States Department of Agriculture, SpO2: saturated peripheral oxygen, CAGR: Compound Annual Growth Rate.
References
- 1.Hydari MZ, Adjerid I, Striegel A. Health Wearables, Gamification, and Healthful Activity. SSRN Electron J. 2019. [Google Scholar] [PubMed]
- 2.Piwek L, Ellis DA, Andrews S, Joinson A. The Rise of Consumer Health Wearables: Promises and Barriers. PLOS Med. 2016;13(2):e1001953. [Google Scholar] [PubMed]
- 3.McCallum C, Rooksby J, Gray CM. Evaluating the Impact of Physical Activity Apps and Wearables: Interdisciplinary Review. JMIR mHealth uHealth 2018;6(3):e58. [Google Scholar] [PubMed]
- 4.Smuck M, Odonkor CA, Wilt JK, Schmidt N, Swiernik MA. The emerging clinical role of wearables: factors for successful implementation in healthcare. npj Digit Med. 2021;4(1):45. [Google Scholar] [PubMed]
- 5.Hilty DM, Armstrong CM, Luxton DD, Gentry MT, Krupinski EA. A Scoping Review of Sensors, Wearables, and Remote Monitoring For Behavioral Health: Uses, Outcomes, Clinical Competencies, and Research Directions. J Technol Behav Sci. 2021;6(2):278–313. [Google Scholar] [PubMed]
- 6.Baxendale G. Health Wearables. ITNOW. 2016 ;58(3):42–3. [Google Scholar] [PubMed]
- 7.Witt DR, Kellogg RA, Snyder MP, Dunn J. Windows into human health through wearables data analytics. Curr Opin Biomed Eng. 2019;9:28–46. [Google Scholar] [PubMed]
- 8.Tully J, Dameff C, Longhurst CA. Wave of Wearables. Clin Lab Med. 2020;40(1):69–82. [Google Scholar] [PubMed]
- 9.Jaén-Carrillo D, Roche-Seruendo LE, Cartón-Llorente A, Ramírez-Campillo R, García-Pinillos F. Mechanical Power in Endurance Running: A Scoping Review on Sensors for Power Output Estimation during Running. Sensors. 2020;20(22):6482. [Google Scholar] [PubMed]
- 10.Wei J. How Wearables Intersect with the Cloud and the Internet of Things : Considerations for the developers of wearables. IEEE Consum Electron Mag. 2014;3(3):53–6. [Google Scholar] [PubMed]
- 11.Chen Y-H, Sawan M. Trends and Challenges of Wearable Multimodal Technologies for Stroke Risk Prediction. Sensors. 2021;21(2):460. [Google Scholar] [PubMed]
- 12.Asimakopoulos S, Asimakopoulos G, Spillers F. Motivation and User Engagement in Fitness Tracking: Heuristics for Mobile Healthcare Wearables. Informatics. 2017;4(1):5. [Google Scholar] [PubMed]
- 13.Knowles B, Smith-Renner A, Poursabzi-Sangdeh F, Lu D, Alabi H. Uncertainty in current and future health wearables. Commun ACM. 2018;61(12):62–7. [Google Scholar] [PubMed]
- 14.Ameli J. Communicable diseases and outbreak control. Vol. 15, Turkish Journal of Emergency Medicine. 2015. p. 20–6. [Google Scholar] [PubMed]
- 15.Kataria I, Siddiqui M, Gillespie T, Goodman M, Dhillon PK, Bann C, et al. A research agenda for non- communicable disease prevention and control in India. Heal Res Policy Syst. 2020;18(1):126. [Google Scholar] [PubMed]
- 16.HabibiSaravi R, Seyedin H, Mosadegh Rad A, Mehdi Gouya M. Communicable diseases management in disasters: an analysis of improvement measures since 2005, Islamic Republic of Iran. East Mediterr Heal J. 2019;25(4):269–81. [Google Scholar] [PubMed]
- 17.Ismail SA, Abbara A, Collin SM, Orcutt M, Coutts AP, Maziak W, et al. Communicable disease surveillance and control in the context of conflict and mass displacement in Syria. Int J Infect Dis. 2016 Jun;47:15–22. [Google Scholar] [PubMed]
- 18.hah B, Mathur P. Research Priorities for Prevention and Control of Noncommunicable Diseases in India. Indian J Community Med. 2011;36(5):72. [Google Scholar] [PubMed]
- 19.Anser MK, Yousaf Z, Khan MA, Nassani AA, Alotaibi SM, Qazi Abro MM, et al. Does communicable diseases (including COVID-19) may increase global poverty risk? A cloud on the horizon. Environ Res. 2020;187:109668. [Google Scholar] [PubMed]
- 20.Modesti PA, Wang J, Damasceno A, Agyemang C, Van Bortel L, Persu A, et al. Indirect implications of COVID- 19 prevention strategies on non-communicable diseases. BMC Med. 2020;18(1):256. [Google Scholar] [PubMed]
- 21.Wang Y, Wang J. Modelling and prediction of global non-communicable diseases. BMC Public Health. 2020;20(1):822. [Google Scholar] [PubMed]
- 22.Luna F, Luyckx VA. Why have Non-communicable Diseases been Left Behind? Asian Bioeth Rev. 2020;12(1):5–25. [Google Scholar] [PubMed]
- 23.Blundell HJ, Hine P. Non-communicable diseases: ditch the label and recapture public awareness. Int Health. 2019;11(1):5–6. [Google Scholar] [PubMed]
- 24.Kam-Tao Li P, Garcia-Garcia G, Lui S-F, Andreoli S, Fung WW-S, Hradsky A, et al. Kidney health for everyone everywhere from prevention to detection and equitable access to care. Nephrol. 2020;24(2):9–21. [Google Scholar] [PubMed]
- 25.Shorey S, Ng ED. The Lived Experiences of Children and Adolescents with Non-Communicable Disease: A Systematic Review of Qualitative Studies. J Pediatr Nurs. 2020;51:75–84. [Google Scholar] [PubMed]
- 26.Herwald H, Egesten A. Who is WHO? J Innate Immun. 2020;12(6):435–6. [Google Scholar] [PubMed]
- 27.Tiwari U, Bano A, Ahmad Khan MK. A review on the COVID-19: Facts and current situation. NeuroPharmac J. 2021;06:180–91. [Google Scholar] [PubMed]
- 28.Tiwari U, Bano A, Ahmad Khan MK. A review on the COVID-19: Facts and current situation. NeuroPharmac J. 2021;06:180–91. [Google Scholar] [PubMed]
- 29.Gherghescu I, Delgado-Charro MB. The Biosimilar Landscape: An Overview of Regulatory Approvals by the EMA and FDA. Pharmaceutics. 2020;13(1):48. [Google Scholar] [PubMed]
- 30.Van Norman GA. Drugs, Devices, and the FDA: Part 1. JACC Basic to Transl Sci. 2016;1(3):170–9. [Google Scholar] [PubMed]
- 31.Gassman AL, Nguyen CP, Joffe H V. FDA Regulation of Prescription Drugs. Campion EW, editor. N Engl J Med. 2017;376(7):674–82. [Google Scholar] [PubMed]
- 32.Ahmad A, Rasul T, Yousaf A, Zaman U. Understanding Factors Influencing Elderly Diabetic Patients’ Continuance Intention to Use Digital Health Wearables: Extending the Technology Acceptance Model (TAM). J Open Innov Technol Mark Complex. 2020;6(3):81. [Google Scholar] [PubMed]
- 33.Kumari KA, Sadasivam GS, Akash SA. A Secure Android Application with Integration of Wearables for Healthcare Monitoring System Using 3D ECCDH PAKE Protocol. J Med Imaging Heal Informatics. 2016;6(6):1548–51. [Google Scholar] [PubMed]
- 34.Mirmomeni M, Fazio T, von Cavallar S, Harrer S. From wearables to THINKables: artificial intelligence- enabled sensors for health monitoring. In: Wearable Sensors. Elsevier; 2021:339–56. [Google Scholar] [PubMed]
- 35.Sivathanu B. Adoption of internet of things (IOT) based wearables for healthcare of older adults – a behavioural reasoning theory (BRT) approach. J Enabling Technol. 2018;12(4):169–85. [Google Scholar] [PubMed]
- 36.Ng K, Ryba T. The Quantified Athlete: Associations of Wearables for High School Athletes. Adv Human- Computer Interact. 2018;2018:1–8. [Google Scholar] [PubMed]
- 37.Henriksen A, Haugen Mikalsen M, Woldaregay AZ, Muzny M, Hartvigsen G, Hopstock LA, et al. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J Med Internet Res. 2018;20(3):e110. [Google Scholar] [PubMed]
- 38.Düking P, Fuss FK, Holmberg H-C, Sperlich B. Recommendations for Assessment of the Reliability, Sensitivity, and Validity of Data Provided by Wearable Sensors Designed for Monitoring Physical Activity. JMIR mHealth uHealth. 2018;6(4):e102. [Google Scholar] [PubMed]
- 39.Alves T, Deroco P, Wachholz Junior D, Vidotto L, Kubota L. Wireless Wearable Electrochemical Sensors: A Review. Brazilian J Anal Chem. 2021;8. [Google Scholar] [PubMed]
- 40.Xia X, Mugo SM, Zhang Q. Responsive microgels-based wearable devices for sensing multiple health signals. Chem Eng J. 2022;427:130903. [Google Scholar] [PubMed]
- 41.An BW, Shin JH, Kim S-Y, Kim J, Ji S, Park J, et al. Smart Sensor Systems for Wearable Electronic Devices. Polymers (Basel). 2017;9(12):303. [Google Scholar] [PubMed]
- 42.Sperlich B, Aminian K, Düking P, Holmberg H-C. Editorial: Wearable Sensor Technology for Monitoring Training Load and Health in the Athletic Population. Front Physiol. 2019;10:1520. [Google Scholar] [PubMed]
- 43.Donisi L, Cesarelli G, Coccia A, Panigazzi M, Capodaglio EM, D’Addio G. Work-Related Risk Assessment According to the Revised NIOSH Lifting Equation: A Preliminary Study Using a Wearable Inertial Sensor and Machine Learning. Sensors. 2021;21(8):2593. [Google Scholar] [PubMed]
- 44.Azodo I, Williams R, Sheikh A, Cresswell K. Opportunities and Challenges Surrounding the Use of Data From Wearable Sensor Devices in Health Care: Qualitative Interview Study. J Med Internet Res. 2020;22(10):e19542. [Google Scholar] [PubMed]
- 45.Muzny M, Henriksen A, Giordanengo A, Muzik J, Grøttland A, Blixgård H, et al. Dataset of wearable sensors with possibilities for data exchange. Data Br. 2020;28:104978. [Google Scholar] [PubMed]
- 46.Picerno P, Iosa M, D’Souza C, Benedetti MG, Paolucci S, Morone G. Wearable inertial sensors for human movement analysis: a five-year update. Expert Rev Med Devices. 2021;18(sup1):79–94. [Google Scholar] [PubMed]
- 47.Muzny M, Henriksen A, Giordanengo A, Muzik J, Grøttland A, Blixgård H, et al. Dataset of wearable sensors with possibilities for data exchange. Data Br. 2020;28:104978. [Google Scholar] [PubMed]
- 48.Zhao P, Ise H, Hongo M, Ota M, Konishi I, Nikaido T. Human Amniotic Mesenchymal Cells Have Some Characteristics of Cardiomyocytes. Transplantation. 2005 Mar 15;79(5):528–35. Dias D, Paulo Silva Cunha J. Wearable Health Devices—Vital Sign Monitoring, Systems and Technologies. Sensors. 2018;18(8):2414. [Google Scholar] [PubMed]
- 49.Luna-Perejón F, Domínguez-Morales MJ, Civit-Balcells A. Wearable Fall Detector Using Recurrent Neural Networks. Sensors. 2019;19(22):4885. [Google Scholar] [PubMed]
- 50.Chander H, Burch RF, Talegaonkar P, Saucier D, Luczak T, Ball JE, et al. Wearable Stretch Sensors for Human Movement Monitoring and Fall Detection in Ergonomics. Int J Environ Res Public Health. 2020;17(10):3554. [Google Scholar] [PubMed]
- 51.Li Z, Zheng Q, Wang ZL, Li Z. Nanogenerator-Based Self-Powered Sensors for Wearable and Implantable Electronics. Research. 2020;2020:1–25. [Google Scholar] [PubMed]
- 52.Xu C, Yang Y, Gao W. Skin-Interfaced Sensors in Digital Medicine: from Materials to Applications. Matter. 2020;2(6):1414–45. [Google Scholar] [PubMed]
- 53.Kim JW, Moon S-M, Kang S, Jang B. Effective Privacy-Preserving Collection of Health Data from a User’s Wearable Device. Appl Sci. 2020;10(18):6396. [Google Scholar] [PubMed]
- 54.Kerner C, Burrows A, McGrane B. Health wearables in adolescents: implications for body satisfaction, motivation and physical activity. Int J Heal Promot Educ. 2019;57(4):191–202. [Google Scholar] [PubMed]
- 55.Greenfield R, Busink E, Wong CP, Riboli-Sasco E, Greenfield G, Majeed A, et al. Truck drivers’ perceptions on wearable devices and health promotion: a qualitative study. BMC Public Health. 2016;16(1):677. [Google Scholar] [PubMed]
- 56.Riva C by: G. DOREMI: Smart Devices and Applications for Healthy Aging. Cyberpsychology, Behav Soc Netw. 2017;20(4):275–6. [Google Scholar] [PubMed]
- 57.Vijayalakshmi K, Uma S, Bhuvanya R, Suresh A. A demand for wearable devices in health care. Int J Eng Technol. 2018;7(1.7):1. [Google Scholar] [PubMed]
- 58.Lu L, Zhang J, Xie Y, Gao F, Xu S, Wu X, et al. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR mHealth uHealth. 2020;8(11):e18907. [Google Scholar] [PubMed]
- 59.Tahri Sqalli M, Al-Thani D. Evolution of Wearable Devices in Health Coaching: Challenges and Opportunities. Front Digit Heal. 2020;2. [Google Scholar] [PubMed]
- 60.Wen D, Zhang X, Lei J. Consumers’ perceived attitudes to wearable devices in health monitoring in China: A survey study. Comput Methods Programs Biomed. 2017;140:131–7. [Google Scholar] [PubMed]
- 61.Stepanovic S, Mettler T, Schmidt-Kraepelin M, Thiebes S, Sunyaev A. Wearable health devices in the workplace: The importance of habits to sustain the use. In: 2019 IEEE 21st Conference on Business Informatics (CBI). IEEE; 2019. p. 363–72. [Google Scholar] [PubMed]
- 62.Konty KJ, Bradshaw B, Ramirez E, Lee W-N, Signorini A, Foschini L. Influenza Surveillance Using Wearable Mobile Health Devices. Online J Public Health Inform. 2019;11(1). [Google Scholar] [PubMed]
- 63.Jo A, Coronel BD, Coakes CE, Mainous AG. Is There a Benefit to Patients Using Wearable Devices Such as Fitbit or Health Apps on Mobiles? A Systematic Review. Am J Med. 2019 Dec;132(12):1394-1400.e1. [Google Scholar] [PubMed]
- 64.Choi B, Hwang S, Lee S. What drives construction workers’ acceptance of wearable technologies in the workplace?: Indoor localization and wearable health devices for occupational safety and health. Autom Constr. 2017;84:31–41. [Google Scholar] [PubMed]
- 65.Zhou Z, Yu H, Shi H. Human Activity Recognition Based on Improved Bayesian Convolution Network to Analyze Health Care Data Using Wearable IoT Device. IEEE Access. 2020;8:86411–8. [Google Scholar] [PubMed]
- 66.Karmen CL, Reisfeld MA, McIntyre MK, Timmermans R, Frishman W. The Clinical Value of Heart Rate Monitoring Using an Apple Watch. Cardiol Rev. 2019;27(2):60–2. [Google Scholar] [PubMed]
- 67.Cappon G, Acciaroli G, Vettoretti M, Facchinetti A, Sparacino G. Wearable Continuous Glucose Monitoring Sensors: A Revolution in Diabetes Treatment. Electronics. 2017;6(3):65. [Google Scholar] [PubMed]
- 68.Dincer C, Bruch R, Costa-Rama E, Fernández-Abedul MT, Merkoçi A, Manz A, et al. Disposable Sensors in Diagnostics, Food, and Environmental Monitoring. Adv Mater. 2019;31(30):1806739. [Google Scholar] [PubMed]
- 69.Casilari E, Álvarez-Marco M, García-Lagos F. A Study of the Use of Gyroscope Measurements in Wearable Fall Detection Systems. Symmetry (Basel). 2020;12(4):649. [Google Scholar] [PubMed]
- 70.Ancans A, Greitans M, Cacurs R, Banga B, Rozentals A. Wearable Sensor Clothing for Body Movement Measurement during Physical Activities in Healthcare. Sensors.;21(6):2068. [Google Scholar] [PubMed]
- 71.Yamamoto Y, Yamamoto D, Takada M, Naito H, Arie T, Akita S, et al. Efficient Skin Temperature Sensor and Stable Gel-Less Sticky ECG Sensor for a Wearable Flexible Healthcare Patch. Adv Healthc Mater. 2017;6(17):1700495. [Google Scholar] [PubMed]
- 72.Kinnunen H, Rantanen A, Kenttä T, Koskimäki H. Feasible assessment of recovery and cardiovascular health: accuracy of nocturnal HR and HRV assessed via ring PPG in comparison to medical grade ECG. Physiol Meas. 2020 Apr 1;41(4):04NT01. [Google Scholar] [PubMed]
- 73.Yin S, Kim M, Kadetotad D, Liu Y, Bae C, Kim SJ, et al. A 1.06-μ W Smart ECG Processor in 65-nm CMOS for Real-Time Biometric Authentication and Personal Cardiac Monitoring. IEEE J Solid-State Circuits. 2019 Aug;54(8):2316–26. [Google Scholar] [PubMed]
- 74.Alizadeh Meghrazi M, Tian Y, Mahnam A, Bhattachan P, Eskandarian L, Taghizadeh Kakhki S, et al. Multichannel ECG recording from waist using textile sensors. Biomed Eng Online. 2020;19(1):48. [Google Scholar] [PubMed]
- 75.Dubosson F, Ranvier J-E, Bromuri S, Calbimonte J-P, Ruiz J, Schumacher M. The open D1NAMO dataset: A multi-modal dataset for research on non-invasive type 1 diabetes management. Informatics Med Unlocked. 2018;13:92–100. [Google Scholar] [PubMed]
- 76.Abdolkhani R, Gray K, Borda A, DeSouza R. Quality Assurance of Health Wearables Data: Participatory Workshop on Barriers, Solutions, and Expectations. JMIR mHealth uHealth. 2020;8(1):e15329. [Google Scholar] [PubMed]
- 77.Kinast B, Lutz M, Schreiweis B. Telemonitoring of Real-World Health Data in Cardiology: A Systematic Review. Int J Environ Res Public Health. 2021;18(17):9070. [Google Scholar] [PubMed]
- 78.Jiang D, Shi G. Research on Data Security and Privacy Protection of Wearable Equipment in Healthcare. Gao Y, editor. J Healthc Eng. 2021 Feb 5;2021:1–7. [Google Scholar] [PubMed]
- 79.Kim JW, Moon S-M, Kang S, Jang B. Effective Privacy-Preserving Collection of Health Data from a User’s Wearable Device. Appl Sci. 2020;10(18):6396. [Google Scholar] [PubMed]
- 80.Kumari V, Hook SA. The Privacy, Security and Discoverability of Data on Wearable Health Devices: Fitness or Folly? In: Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). 2017. p. 50–64. [Google Scholar] [PubMed]
- 81.Wu J, Li H, Lin Z, Goh K-Y. How big data and analytics reshape the wearable device market – the context of e-health. Int J Prod Res. 2017;55(17):5168–82. [Google Scholar] [PubMed]
- 82.Mahloko L, Adebesin F. A Systematic Literature Review of the Factors that Influence the Accuracy of Consumer Wearable Health Device Data. In: Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). 2020:96–107. [Google Scholar] [PubMed]
- 83.Mühlen JM, Stang J, Lykke Skovgaard E, Judice PB, Molina-Garcia P, Johnston W, et al. Recommendations for determining the validity of consumer wearable heart rate devices: expert statement and checklist of the INTERLIVE Network. Br J Sports Med. 2021;55(14):767–79. [Google Scholar] [PubMed]
- 84.Yingling LR, Mitchell V, Ayers CR, Peters-Lawrence M, Wallen GR, Brooks AT, et al. Adherence with physical activity monitoring wearable devices in a community-based population: observations from the Washington, D.C., Cardiovascular Health and Needs Assessment. Transl Behav Med. 2017;7(4):719–30. [Google Scholar] [PubMed]
- 85.Ward NG. A Big-Data Approach. In: Prosodic Patterns in English Conversation. Cambridge University Press; 2019:109–28. [Google Scholar] [PubMed]
- 86.Nelson BW, Low CA, Jacobson N, Areán P, Torous J, Allen NB. Guidelines for wrist-worn consumer wearable assessment of heart rate in biobehavioral research. npj Digit Med. 2020;3(1):90. [Google Scholar] [PubMed]
- 87.Chou L-W, Shen J-H, Lin H-T, Yang Y-T, Hu W-P. A Study on the Influence of Number/Distribution of Sensing Points of the Smart Insoles on the Center of Pressure Estimation for the Internet of Things Applications. Sustainability. 2021;13(5):2934. [Google Scholar] [PubMed]
- 88.Asadi S, Abdullah R, Safaei M, Nazir S. An Integrated SEM-Neural Network Approach for Predicting Determinants of Adoption of Wearable Healthcare Devices. Mob Inf Syst. 2019;2019:1–9. [Google Scholar] [PubMed]
- 89.Lublin FD, Bowen JD, Huddlestone J, Kremenchutzky M, Carpenter A, Corboy JR, et al. Human placenta- derived cells (PDA-001) for the treatment of adults with multiple sclerosis: A randomized, placebo- controlled, multiple-dose study. Mult Scler Relat Disord. 2014 Nov;3(6):696–704.Kooman JP, Wieringa FP, Han M, Chaudhuri S, van der Sande FM, Usvyat LA, et al. Wearable health devices and personal area networks: can they improve outcomes in haemodialysis patients? Nephrol Dial Transplant. 2020;35(Supplement_2):ii43–50. [Google Scholar] [PubMed]
- 90.SBinyamin SS, Hoque MR. Understanding the Drivers of Wearable Health Monitoring Technology: An Extension of the Unified Theory of Acceptance and Use of Technology. Sustainability. 2020;12(22):9605. [Google Scholar] [PubMed]
- 91.Takei K, Honda W, Harada S, Arie T, Akita S. Toward Flexible and Wearable Human-Interactive Health- Monitoring Devices. Adv Healthc Mater. 2015;4(4):487–500. [Google Scholar] [PubMed]
- 92.Riva C by: G. DOREMI: Smart Devices and Applications for Healthy Aging. Cyberpsychology, Behav Soc Netw. 2017;20(4):275–6. [Google Scholar] [PubMed]
- 93.Tu J, Torrente-Rodríguez RM, Wang M, Gao W. The Era of Digital Health: A Review of Portable and Wearable Affinity Biosensors. Adv Funct Mater. 2020;30(29):1906713. [Google Scholar] [PubMed]
- 94.Shan R, Ding J, Weng D, Spaulding EM, Wongvibulsin S, Lee MA, et al. Early blood pressure assessment after acute myocardial infarction: Insights using digital health technology. Am J Prev Cardiol. 2020;3:100089. [Google Scholar] [PubMed]
- 95.Dharmik RC, Gotarkar S, Dinesh P, Sant Burde H. An IoT Framework for Healthcare Monitoring System. J Phys Conf Ser. 2021;1913(1):012145. [Google Scholar] [PubMed]
- 96.Sharma A, Badea M, Tiwari S, Marty JL. Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring. Molecules. 2021;26(3):748. [Google Scholar] [PubMed]
- 97.Lee SY, Lee K. Factors that influence an individual’s intention to adopt a wearable healthcare device: The case of a wearable fitness tracker. Technol Forecast Soc Change. 2018;129:154–63. [Google Scholar] [PubMed]
- 98.Pardamean B, Soeparno H, Budiarto A, Mahesworo B, Baurley J. Quantified Self-Using Consumer Wearable Device: Predicting Physical and Mental Health. Healthc Inform Res. 2020;26(2):83–92. [Google Scholar] [PubMed]
- 99.Marrouche NF. New Consumer Guidance on Wearable Devices from the Consumer Electronics Show 2020. Heart Int. 2020;14(1):9. [Google Scholar] [PubMed]
- 100.Aydin MN, Perdahci NZ. Dynamic network analysis of online interactive platform. Inf Syst Front. 2019;21(2):229–40. [Google Scholar] [PubMed]
- 101.Khanwalkar AR, Shen J, Kern RC, Welch KC, Smith SS, Tan BK, et al. Utilization of a novel interactive mobile health platform to evaluate functional outcomes and pain following septoplasty and functional endoscopic sinus surgery. Int Forum Allergy Rhinol. 2019;9(4):345–51. [Google Scholar] [PubMed]
- 102.Takei K, Gao W, Wang C, Javey A. Physical and Chemical Sensing With Electronic Skin. Proc IEEE. 2019;107(10):2155–67. [Google Scholar] [PubMed]
- 103.Göransson C, Wengström Y, Ziegert K, Langius-Eklöf A, Eriksson I, Kihlgren A, et al. Perspectives of health and self-care among older persons-To be implemented in an interactive information and communication technology-platform. J Clin Nurs. 2017;26(23–24):4745–55. [Google Scholar] [PubMed]
- 104.Milne-Ives M, Lam C, De Cock C, Van Velthoven MH, Meinert E. Mobile Apps for Health Behavior Change in Physical Activity, Diet, Drug and Alcohol Use, and Mental Health: Systematic Review. JMIR mHealth uHealth. 2020;8(3):e17046. [Google Scholar] [PubMed]
- 105.Lu L, Zhang J, Xie Y, Gao F, Xu S, Wu X, et al. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR mHealth uHealth. 2020;8(11):e18907. [Google Scholar] [PubMed]

